What is a Colonoscopy? [PDF]
Colonoscopy (also known as lower GI endoscopy) is a procedure that enables a Gastroenterologist to examine the lining of the large bowel (colon) using a thin flexible tube with a camera lens and light source. This examination includes the entire length of the large bowel, and often the very last few centimetres of the small bowel. This information sheet will give you a basic understanding of the procedure – how it is performed, how it may help, and what side-effects you might experience. Please ask Dr Fanning about anything you do not understand.
Why is Colonoscopy performed?
Colonoscopy is performed to evaluate a variety of symptoms including lower abdominal pain, a change in bowel habit, weight loss, or rectal bleeding. Colonoscopy is also regularly performed in patients with a personal or family history of bowel cancer. It is the best test for finding a source of bleeding from the lower gastrointestinal tract. Some common causes include:- vascular abnormalities, Crohn’s disease and Ulcerative colitis (inflammation of the bowel wall), haemorrhoids, diverticular disease, ulcers, polyps and tumours of the lower GI tract. Biopsies (small tissue samples) may also be taken at the time of your Colonoscopy. Many conditions can also be treated at the time of Colonoscopy. Examples include dilating narrowed regions, removing polyps, and treating lower gastrointestinal bleeding. Safe and effective endoscopic control of bleeding has reduced the need for transfusions and surgery in many patients.
What are the possible complications of Colonoscopy?
Endoscopy is generally safe and well-tolerated. Complications can occur, but are rare when the test is performed by Physicians with specialised training and experience in the procedure. Risks vary depending on why the test is performed, what is found during the procedure, what therapeutic intervention is undertaken, and whether a patient has underlying major medical problems. Complications can include bleeding, infection, pain, or perforation (a tear in the wall of the bowel). It is rare to have a major complication such as perforation (1:1,000), however if any significant symptoms develop after your procedure please inform Dr Fanning immediately.
Bleeding may occur from biopsy or polypectomy sites, but this is usually minimal and rarely requires additional therapy.
Reactions to the sedatives used and complications from heart or lung diseases, including death, are extremely rare but potential risks.
What can I expect during Colonoscopy?
The bowel must be cleaned of residual faecal material prior to colonoscopy. This entails a modified diet and extensive bowel preparation, which results in a laxative effect. Dr Fanning will discuss this with you, and provide detailed information on how to prepare for the procedure. You must fast for at least four hours prior to the procedure.
You should talk to Dr Fanning about any regular medications that you take, and any known drug allergies. Although an allergy doesn’t prevent you from having a Colonoscopy, it is important to discuss it prior to the procedure. Also, be sure to mention if you have any major diseases, or take regular blood-thinning medications such as Aspirin [Cartia, Solprin], Clopidogrel [Plavix, Iscover], Warfarin [Marevan, Coumadin], Rivaroxaban [Xarelto], Dabigatran [Pradaxa], Ticagrelor [Brilinta], Apixaban [Eliquis], or Prasugrel [Effient].
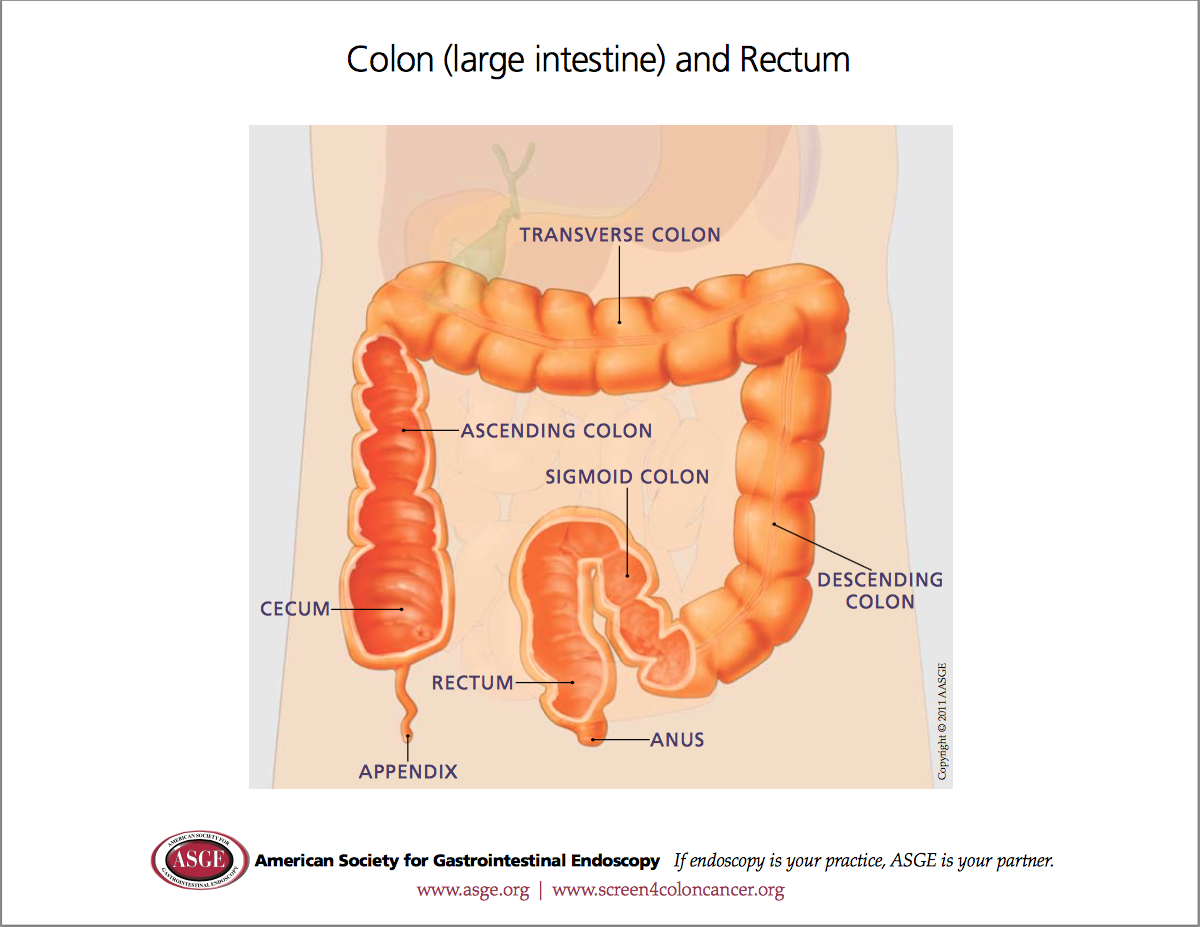
You will lie on your left side during the procedure, with Intravenous sedation used to make you comfortable. The Anaesthetist will ensure you are comfortable, with most patients sleeping through the whole procedure. The colonoscope is then inserted into the anus and gently advanced around the colon. You might feel bloated afterwards because of the air introduced through the instrument.
A detailed examination is performed, and a report written explaining the findings.
What can I expect after Colonoscopy?
After your Colonoscopy you will be observed for complications until most of the effects of the medications have worn off. You might experience bloating or pass gas because of the air introduced during the examination. You should not have any significant pain.
Most patients are to remain fasting for 30 minutes post procedure, and can then resume a normal diet. Those with a large polyp removed are required to remain fasting for 2 hours post procedure, and then continue clear fluids for the remainder of the day.
Dr Fanning will discuss the findings and future plans with you after the procedure.
Someone must accompany you home from the procedure because of the sedatives used during the examination.
Even if you feel alert after the procedure, the sedatives can affect your judgment and reflexes for the rest of the day.
YOU MUST NOT DRIVE OR OPERATE MACHINERY UNTIL THE NEXT DAY.
If you experience any complications after the procedure please contact Dr Fanning immediately, or proceed to the Emergency Department if this occurs after hours or on the weekend.
BOWEL PREPARATION INFORMATION
A number of different bowel preparations are available. The choice of preparation will be determined by discussion prior to your procedure. The links below are for general information only: –