What is an ERCP? [PDF]
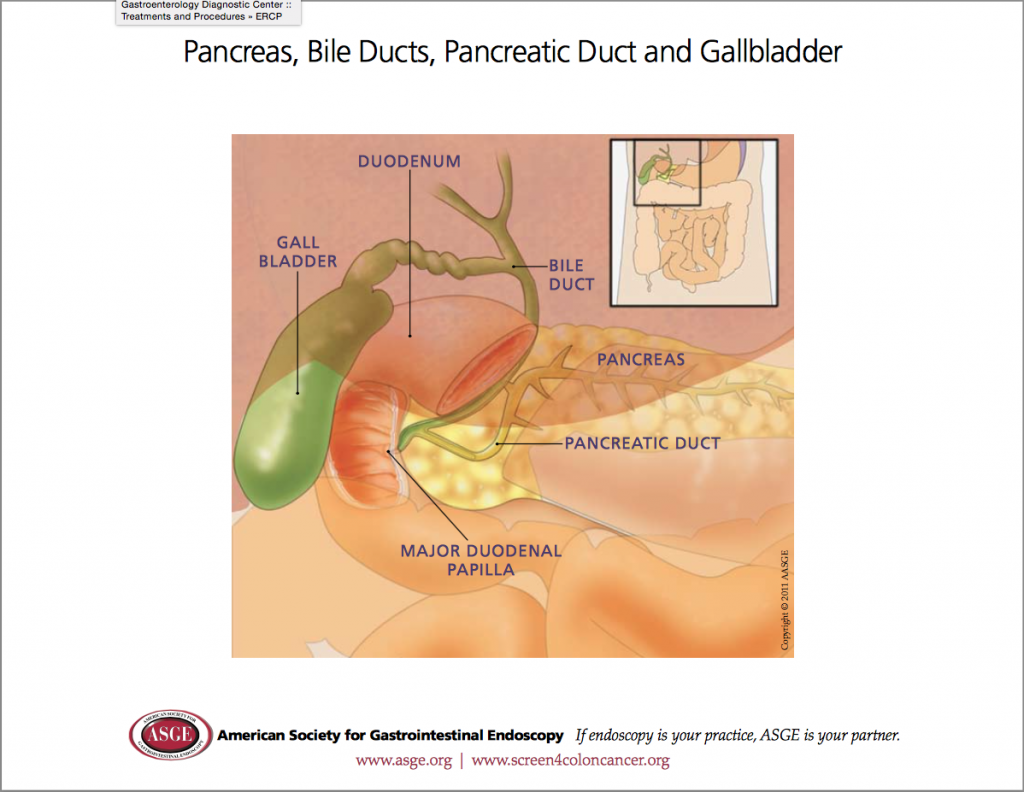
Endoscopic retrograde cholangiopancreatography, or ERCP, is a specialised technique used to study and treat abnormalities of the ducts or “drainage tubes” of the gallbladder, pancreas, and liver. This information sheet will give you a basic understanding of the procedure – how it is performed, how it may help, and what side-effects you might experience. Please ask Dr Fanning about anything you do not understand.
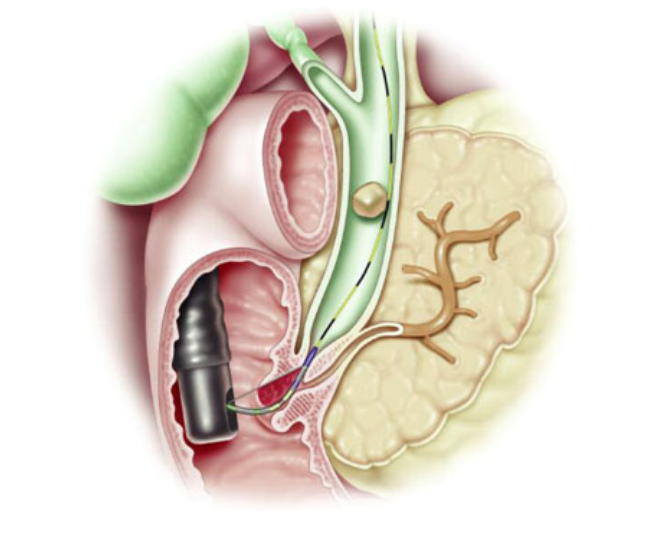
During ERCP, a duodenoscope (a thin, flexible, side-viewing endoscope) is passed through your mouth, past the oesophagus and stomach, and into the first part of the small intestine. A thin guidewire and narrow plastic tube called a sphincterotome is then passed into the ducts. X-ray dye is injected in order to obtain a picture of the ducts. If an abnormality is found, a small incision (sphincterotomy) is usually made along the duct to allow further therapeutic procedures. This may include removal of stone or debris, dilatation of narrowings (strictures), taking a biopsy, and/or insertion of stents (plastic or metal drainage tubes).
What preparation is required?
You must fast for at least 6 hours before the procedure to ensure you have an empty stomach. Generally, you should take all your regular medications with a sip of water, even on the morning of the procedure.
However if you are taking blood-thinning medications (such as Aspirin [Cartia, Solprin], Clopidogrel [Plavix, Iscover], Warfarin [Marevan, Coumadin], Rivaroxaban [Xarelto], Dabigatran [Pradaxa], Ticagrelor [Brilinta], Apixaban [Eliquis], or Prasugrel [Effient]), Dr Fanning will need to discuss whether these should still be taken prior to the procedure. Please mention any allergies you have to medications (including intravenous contrast, Iodine, Shellfish). Although an allergy does not prevent you from having ERCP, it is important to discuss prior to the procedure.
Please advise if you are diabetic or have a pacemaker, as we may need to make special arrangements.
What can I expect during ERCP?
Local anaesthetic spray and intravenous sedation are used to make you comfortable. Some patients also receive antibiotics before the procedure. You will lie on your left side or stomach on an X-ray table. Most patients remember little or none of the procedure. ERCP usually takes around 30 to 45 minutes to perform. The instrument does not interfere with breathing, but you might feel bloated afterwards because of the air introduced.
What are the risks of ERCP?
ERCP is a well-tolerated and safe procedure when performed by Doctors who are specially trained and experienced in the technique. Although complications requiring hospitalisation can occur, they are uncommon. Complications can include pancreatitis (inflammation of the pancreas), infections, perforation, and bleeding. Rarely patients can have an adverse reaction to the sedatives used. ERCP is usually successful, but sometimes cannot be completed for technical reasons. Risks vary depending on why the test is performed, what is found during the procedure, what therapeutic intervention is undertaken, and whether a patient has underlying major medical problems. The most frequent complication is pancreatitis. This occurs after 3-5% of ERCPs. It is very rare (<0.2%) if you have had a previous ERCP with sphincterotomy. Reactions to the sedatives used and complications from heart or lung diseases, including death, are extremely rare but potential risks.
The procedure is usually successful, however there is a 5% chance that it will not be possible to perform due to technical difficulties.
It is important to understand that to solve the clinical problem and cure the illness, in general ERCP carries the lowest risk to the patient when compared with observation alone (doing nothing), surgery, or the radiological approach (going through the liver). After ERCP, more than 95% of patients return to normal activities the next day.
What can I expect after ERCP?
After your ERCP you will be observed for complications until most of the effects of the medications have worn off. You might experience bloating or pass gas because of the air introduced during the examination.
You should not have any significant pain. Dr Fanning will discuss the findings and future plans with you after the procedure.
You will remain fasting for 4 hours post procedure, and must remain on a clear liquid diet until the following day. The next day you should only eat light (non-fatty) food. After that, the diet can be upgraded.
Someone must accompany you home from the procedure because of the sedatives used during the examination.
Even if you feel alert after the procedure, the sedatives can affect your judgment and reflexes for the rest of the day.
YOU MUST NOT DRIVE OR OPERATE MACHINERY UNTIL THE NEXT DAY.
Please contact Dr Fanning if you experience any complications after the procedure. The main complication after going home is pancreatitis, which can occasionally occur up to 48 hours after the procedure. If you develop severe abdominal pain, you may have pancreatitis. Contact Dr Fanning immediately, or proceed to the Emergency Department.