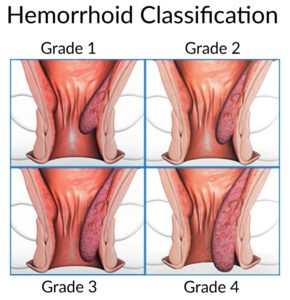
Haemorrhoid banding is a common treatment for grade 2 and 3 haemorrhoids.
- Grade 1 are small swellings on the inside lining of the back passage. They cannot be seen or felt from outside the anus. Grade 1 haemorrhoids are common, and are often asymptomatic. If problematic, they are often responsive to simple remedies such as creams and suppositories. In some people they enlarge over time to grade 2 or more.
- Grade 2 are larger. They may be partly pushed out (prolapse) from the anus when you go to the toilet, but quickly ‘spring back’ inside again.
- Grade 3 hang out (prolapse) from the anus. You may feel one or more as small, soft lumps that hang out from the anus. However, you can push them back inside with a finger.
- Grade 4 permanently hang down from within the anus, and you cannot push them back inside. They sometimes become quite large, and usually require surgery to correct.
 Banding haemorrhoids is usually done at the time of colonoscopy, but can also be performed in an outpatient clinic. The haemorrhoid is grasped with a suction device. A rubber band is placed at the base of the haemorrhoid which then cuts off the blood supply. The haemorrhoid then ‘dies’ and drops off after a few days. The tissue at the base of the haemorrhoid heals with some scar tissue.
Banding haemorrhoids is usually done at the time of colonoscopy, but can also be performed in an outpatient clinic. The haemorrhoid is grasped with a suction device. A rubber band is placed at the base of the haemorrhoid which then cuts off the blood supply. The haemorrhoid then ‘dies’ and drops off after a few days. The tissue at the base of the haemorrhoid heals with some scar tissue.
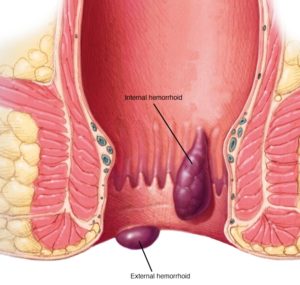
Banding of internal haemorrhoids is usually painless as the base of the haemorrhoid originates above the anal opening (dentate line) – in the very last part of the gut where the gut lining is not sensitive to pain. Several haemorrhoids may be treated at one time using this method. Banding is usually very successful, but sometimes haemorrhoids can recur. If this occurs, further banding treatment is required. Banding does not work in a small number of cases. Haemorrhoids are less likely to recur after banding if you consume plenty of fibre, do not become constipated, and do not strain on the toilet

